Kawsari Abdullah, Jingqin Zhu, Andrea Gershon, Sharon Dell, Teresa To
European Respiratory Journal 2020 55: 1901335; DOI: 10.1183/13993003.01335-2019
Abstract
The association between asthma exacerbation during pregnancy and adverse maternal and child health outcomes have not been investigated appropriately. Our objective was to determine the short- and long-term intergenerational effect of asthma exacerbation in pregnant women with asthma.
A population cohort study was conducted using data from the Ontario asthma surveillance system and population-level health administrative data. Asthma exacerbation in pregnant women with asthma was defined as at least one of the following criteria: at least five physician visits, or one emergency department visit or one hospital admission for asthma during pregnancy. Pregnancy complications, adverse perinatal outcomes and early childhood respiratory disorders were identified using International Classification of Disease codes (9th and 10th revisions).
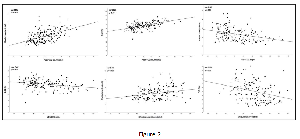
The cohort consisted of 103 424 singleton pregnancies in women with asthma. Asthma exacerbation in pregnant women with asthma was associated with higher odds of pre-eclampsia (OR 1.30, 95% CI 1.12–1.51) and pregnancy-induced hypertension (OR 1.17, 95% CI 1.02–1.33); babies had higher odds of low birthweight (OR 1.14, 95% CI 1.00–1.31), preterm birth (OR 1.14, 95% CI 1.01–1.29) and congenital malformations (OR 1.21, 95% CI 1.05–1.39). Children born to women with asthma exacerbation during pregnancy had elevated risk of asthma (OR 1.23, 95% CI 1.13–1.33) and pneumonia (OR 1.12, 95% CI 1.03–1.22) during the first 5 years of life.
Asthma exacerbation during pregnancy in women with asthma showed increased risk of pregnancy complications, adverse perinatal outcomes and early childhood respiratory disorders in their children, indicating that appropriate asthma management may reduce the risk of adverse health outcomes.
Footnotes
-
This article has supplementary material available from erj.ersjournals.com
-
Conflict of interest: K. Abdullah has nothing to disclose.
-
Conflict of interest: J. Zhu has nothing to disclose.
-
Conflict of interest: A. Gershon has nothing to disclose.
-
Conflict of interest: S. Dell has nothing to disclose.
-
Conflict of interest: T. To has nothing to disclose.
-
Support statement: This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and information compiled and provided by CIHI. However, the analyses, conclusions, opinions and statements expressed herein are those of the author, and not necessarily those of CIHI. Funding information for this article has been deposited with the Crossref Funder Registry.
- Received July 5, 2019.
- Accepted October 24, 2019.
- Copyright ©ERS 2020