Aleksandra Kotwica, Harry Knights, Nikhil Mayor, Emma Russell-Jones, Theodore Dassios, David Russell-Jones
European Respiratory Journal 2020; DOI: 10.1183/13993003.03841-2020
Using simple bedside pulse oximetry to create oxygen-haemoglobin desaturation curves may be useful in triaging patients with COVID-19. Intrapulmonary shunting is associated with worse outcomes in COVID-19, and the degree of shunt appears to predict outcome
Introduction
Hypoxaemia is a key indicator for hospital admission with COVID-19. Controversy surrounds the pathophysiology underlying hypoxaemia, with intrapulmonary shunt, mismatch in ventilation-to-perfusion (VA/Q) ratio, endothelial injury, microvascular coagulation, and host inflammatory response hypothesised to play a role. It has recently been proposed that COVID-19 pneumonia may exist as two phenotypes dependent on the preservation of lung mechanics and the relative contribution of VA/Q mismatch and intrapulmonary shunting to hypoxaemia. We hypothesise that V/Q mismatch and intrapulmonary shunting are present in COVID-19 pneumonia and aimed to assess their effect on outcome. A mathematical model was used to construct oxygen–haemoglobin dissociation curves (ODC) to determine the degree of shunt and VA/Q mismatch in a cohort of patients with severe COVID-19. Factors contributing to shunt and mortality were identified.
Methods
All patients presenting to our hospital in March 2020 with a diagnosis of COVID-19 through real-time PCR were included.
Epidemiological, clinical, laboratory, and radiological characteristics were collected in addition to level of oxygen therapy required and outcome. Unless anticoagulated prior to admission, all patients received venous thromboembolism prophylaxis. The NEWS2 score was used for all patients, a validated aggregate scoring system of patient physiological observations.
We retrospectively collected fingertip pulse oximetry data documented by paramedics and the emergency department. Two saturations at different FiO2 values taken on admission and less than six hours apart were used to construct ODCs. In ten patients, the model was unable to derive a curve for the calculation of Va/Q. This was likely because they deteriorated rapidly on admission, skewing the data. However, the model was still able to calculate intrapulmonary shunt for these patients using a single data point.
The construction of ODCs has been described in detail elsewhere (fig. 1a). The method uses a two-compartment model and corrects for haemoglobin concentration. Shunting reduces arterial oxygen saturation through arteriovenous admixture which cannot be corrected by increasing FiO2. The shunt can therefore be calculated from depression of the ODC. VA/Q reduction decreases post-alveolar blood oxygen content, shifting the ODC rightwards. This is reversible by increasing FiO2. These parameters are quantified by comparison to a reference curve.
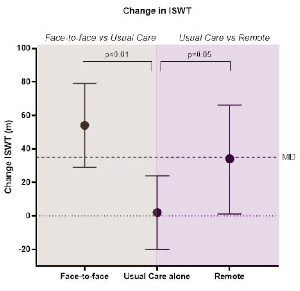
FIGURE 1
a) Ventilation to perfusion ratio in the death and survivor groups. b) Intrapulmonary shunt in the death and survivor groups (%). c) Mortality rate at increasing level of intrapulmonary shunt (%).
Spearman rank correlation co-efficient was used to examine the relationship between shunt and clinical parameters.
Results
In March 2020, 108 patients were admitted with confirmed COVID-19. Fourteen not requiring oxygen and seven without adequate data available were excluded. The remaining 87 were included. Mean age was 68·3±1·8 years and 41% (n=36) were female. Mean BMI was 28·3±0·1 kg·m−2. 65 patients (75%) were white British; 8 (9%) white other; 8 (9%) black, Asian, or minority ethnic (BAME); and 6 (7%) unknown ethnicity. 46% of patients were ex or current smokers. Cardiovascular diseases (hypertension [46%], stroke [16%], ischaemic heart disease [13%]), diabetes (25%) and respiratory diseases (asthma [15%], COPD [15%]) were the most common comorbidities. 24% of patients had previous or current cancer.
Baseline blood tests showed an activated inflammatory response (median CRP 82, IQR 49–156; lactate dehydrogenase 628, 528–807; ferritin 926, 357–1620) and coagulation cascade (median D-dimer 1100, 663–1550). One patient had a possible pulmonary embolus on CTPA in addition to severe COVID-19 changes. Thirty one patients (36%) died.
The median shunt was 14% (IQR 4–21) and VA/Q was 0·58 (IQR 0·50–0·68) (fig. 1a). Shunt was 45% higher (p=0.03) in patients that died (16%, IQR 6–23) than survived (11%, IQR 1–17) (fig. 1b). There was no difference (p=0.69) between the median VA/Q ratio of patients that died (0.59, 0.49–0.70) than survived (0.50 IQR 0.56–0.68) (fig. 2). Mortality rate increased with shunt severity (fig. 1c). All five patients with a shunt greater than 30% died.
Shunt was related to admission NEWS2 score (Spearman correlation coefficient 0.33, p=0.0002), CRP (0.38, p=0.001), LDH (0.45, p=0.002), urea (0.29, p=0.007), as well as duration of CPAP (0.40, p=0.001) and length of hospital stay (0.25, p=0.02). VA/Q mismatch was not related to any measured parameters.
Discussion
The pathophysiology underlying hypoxaemia in COVID-19 is controversial. This study identifies intrapulmonary shunt as a major pathophysiological mechanism. Shunt severity was predictive of worse outcome: length of stay; CPAP duration; and mortality. Furthermore, shunt correlated with CRP and LDH, but not D-dimer. VA/Q mismatch, although present, was not prognostic.
Micro and macrovascular thrombosis within the pulmonary architecture have been implicated in the pathogenesis of COVID-19 hypoxaemia. Dual–energy CT-scans identified profound perfusion abnormalities with shunting of blood to areas of lung with impaired gas exchange . Our study confirms that pulmonary vascular shunting may play a significant role in the development of hypoxaemia in COVID-19. From a pathophysiological perspective, the strong correlation of CRP with intrapulmonary shunt and outcomes such as length of CPAP and death implies that a more profound inflammatory response correlates with more severe shunting, which in turn is related to worse clinical outcomes.
It has been hypothesised that COVID-19 pneumonia may exist on a spectrum between two phenotypes. The less severe form (“Type L”) may be associated with preserved lung mechanics with hypoxia proposed to be secondary to localised pulmonary vascular inflammation impairing hypoxic pulmonary vasoconstriction and physiological ventilation-perfusion matching. The more severe form (“Type H”) may be associated with a more “typical” acute respiratory distress syndrome (ARDS) picture: reduced lung compliance, enhanced inflammation, and shunting. This theoretical model was derived from clinician observation and, to date, has not been formally confirmed. Our study provides evidence in favour of this hypothesis by confirming that more severe shunting is associated with worse outcomes, whilst VA/Q mismatching does not correlate with severity of disease. The pathophysiology underlying a shunt means hypoxaemia cannot be completely reversed by increasing FiO2. This may provide an explanation for why these patients have worse outcomes. Further research may also provide insight into the underlying mechanisms responsible for “silent hypoxia” described in COVID-19 and the role of intrapulmonary shunting.
This study also demonstrates that oxygen saturations at two different FiO2 values can be used to construct ODCs useful for predicting outcome. A simple computer-based algorithm was used that can be performed at the bedside on admission and may help prioritise treatment pathways. The strength of this method is that the ODC is a predictable physical property of haemoglobin which even in fluctuating clinical situations allows the objective and accurate measurement of shunting and VA/Q mismatch. It performs well against more complex methods.
This study is limited by the small sample size. However, numbers are in excess of studies using this technique in other clinical conditions . Furthermore, the retrospective design means that oxygen saturations were taken up to six hours apart. Future prospective studies will be able to collect oxygen saturations at different FiO2 in a shorter time period, reducing the risk of patient deterioration in the interval period.
This study highlights the utility of simple clinical measurements to construct an ODC quantifying shunt and VA/Q mismatch in patients with COVID-19. We also show that the degree of shunt appears to predict outcome. Furthermore, these observations add to our understanding of the pathophysiological mechanisms responsible for hypoxaemia in COVID-19. Our study has significant clinical applicability. Our non-invasive method of early calculation of shunt could assist decisions on triaging and risk stratifying. Given, though, the limited number of subjects and retrospective nature of our study, the next phase of our research will aim to validate these results in a larger, prospective cohort.
Acknowledgments
We sincerely thank all the doctors, nurses, and health care staff involved in the management of patients with COVID-19 at the Royal Surrey NHS Foundation Trust.
Footnotes
-
Ethics and informed consent: The study was approved by the local Patient Safety and Quality Control Committee. The Medical Research Council ethics decision tool indicates that this research does not require review by an NHS Research Ethics Committee in England. As all patient data was anonymised, informed consent was not deemed necessary for this study, in line with local guidance.
-
Contributors: AK, HK, NM, ERJ, and DRJ drafted the manuscript. AK, TD, and HK performed the data analysis. All authors contributed to study conception and design, revision of the manuscript, data collection, and patient enrolment. DRJ is corresponding author, had access to all the data in the study, and had final responsibility for the decision to submit for publication.
Patient and public involvement: A patient advisory group consisting of four current inpatients not included in the study cohort commented on the findings and contributed to the discussion and dissemination plan.
-
Support statement: None.
-
Conflict of interest: Dr. Kotwica has nothing to disclose.
-
Conflict of interest: Dr. Knights has nothing to disclose.
-
Conflict of interest: Dr. Mayor has nothing to disclose.
-
Conflict of interest: Professor Russell-Jones has nothing to disclose.
-
Conflict of interest: Dr. Dassios has nothing to disclose.
-
Conflict of interest: Dr. Russell-Jones has nothing to disclose.
- Received October 13, 2020.
- Accepted November 26, 2020.
- Copyright ©ERS 2020