Abstract
Background
The carbon footprint of severe asthma and the impact of biologic therapy in this population is unknown.
Methods
This was a retrospective cohort study in adults with severe asthma, using data from the Northern Ireland Regional Severe Asthma Service (September 2015–November 2021). We calculated annual greenhouse gas (GHG) emissions (carbon dioxide equivalent) for asthma-related medications and healthcare resource utilisation, compared patient characteristics by GHG quartile, calculated GHG change post-biologic initiation, and explored the relationship between GHG change and clinical response.
Results
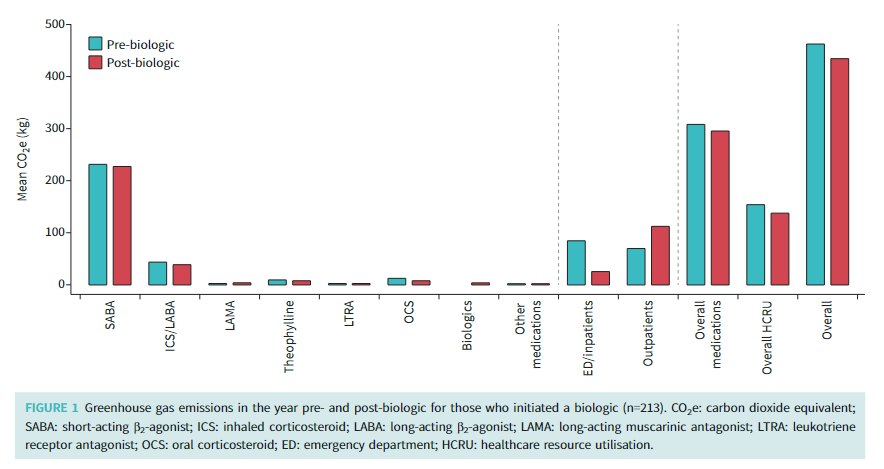
Among 303 patients with severe asthma, mean±sd GHG emissions were 474±431 kg, largely driven by SABA use (50.7%) and emergency department (ED) visits/inpatient admissions (21.0%). Those with highest-quartile GHG emissions were more likely to have uncontrolled disease (Asthma Control Questionnaire-5 score 3.5 versus 2.5; p<0.001), be more deprived (46.1% versus 25.0%; p=0.029) and have depression/anxiety (35.5% versus 14.7%; p=0.002) versus those with lowest-quartile GHG emissions. Among patients who received a biologic (n=213), modest GHG reductions (−28.0±286 kg; p=0.15) were observed, largely driven by a reduction in ED/hospitalisation-related GHG emissions (−59.3±224 kg; p<0.001). SABA-related GHG emissions were relatively unchanged (−6.1±138 kg; p=0.518). Total GHG emissions were 72.4±352 kg (p=0.044) lower than baseline at 4 years post-biologic initiation. Although there was substantial clinical improvement post-biologic initiation, this was not associated with GHG reductions.
Conclusions
Severe asthma is associated with substantial GHG emissions, primarily driven by SABA use and emergency care utilisation. Although GHG emissions were lower post-biologic, largely due to a reduction in emergency care, the changes in GHG emissions were modest and SABA use was relatively unchanged. An improved understanding of the factors driving elevated GHG emissions is required.














