Abstract
Background
The clinical impact of bacterial and mycobacterial isolates on bronchiectasis remains uncertain.
Materials and methods
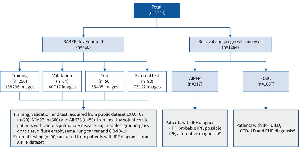
Patients with bronchiectasis at 16 hospitals in Taiwan were recruited with a 1-year follow-up. The patients were classified into six groups: Group 1, Pseudomonas aeruginosa; Group 2, Klebsiella pneumoniae; Group 3, Other bacteria; Group 4, Non-tuberculous mycobacteria (NTM); Group 5, Daily sputum without bacterial or NTM colonization; and Group 6, Dry bronchiectasis.
Results
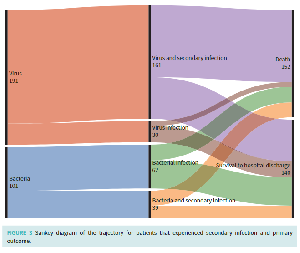
A total of 1416 patients (mean age, 67?years; males, 43%) were included. The mean modified Reiff score was 5 (range: 1–18). Fifty-nine percent (829 patients) had sputum, whereas the remaining did not. The proportions of bacteria and NTM cultured from sputum within one year of observation were 27% (381/1416) and 15% (202/1416), respectively. The most common bacterial isolate was P. aeruginosa (13%), followed by K. pneumoniae (7%). Twenty-six percent of the patients experienced severe exacerbations at least once within the year. The one-year all-cause mortality rate was 3%. Patients with sputum exhibited a higher rate of severe exacerbations compared to that in patients with dry bronchiectasis, regardless of the presence of bacteria or NTM (p<0·001). Patients with bacterial colonization had a higher mortality rate (p<0·001). Further, the highest mortality rate was observed among those with K. pneumoniae colonization (hazard ratio [HR]: 8.39, 95% confidence interval [95% CI]: 2.39–29.49), followed by individuals colonized with other bacteria (HR: 8.04, 95% CI: 2.36–27.38) and P. aeruginosa (HR: 7.83, 95% CI: 2.45–25.03). Additionally, old age was an independent risk factor (HR, 2.72; 95% CI: 1.19–6.18).
Conclusion
K. pneumoniae was more frequently isolated from patients with bronchiectasis in Taiwan, compared with Western countries and was associated with unfavorable clinical outcomes.